Abstract
INTRODUCTION
Diagnosing acquired haemophilia A (AHA) can be challenging due to a) it's rarity (~1.5 cases per million), and b) the range of nonspecific bleeding patterns that may present. Therefore, there is a substantial diagnostic delay and rate of misdiagnosis, leading to an increased risk of morbidity and mortality.
This study was conducted to determine whether online interactive case-based independent medical education could improve clinicians' competence in identifying possible AHA, in appropriate referral to specialist centers and in initial management.
METHODS
Hematologists and emergency medicine (EM) physicians participated in a text, case-based activity and completed pre- and post-questions (Ma A. Active Bleeding in the ER and a Prolonged aPTT: What's Your Next Step? www.medscape.org/viewarticle/944112). Educational effect was assessed using a 3-question repeated-pair design with pre-/post-assessment. A paired samples t-test was conducted for significance testing on overall average number of correct responses and for confidence rating, and a McNemar's test was conducted at the learning objective level (5% significance level, P <.05). Cohen's d with correction for paired samples estimated the effect size of the education on number of correct responses (<.20 modest, .20-.49 small, .59-.79 moderate, ≥.80 large). Data were collected from 03/15/2021 to 06/14/2021.
RESULTS
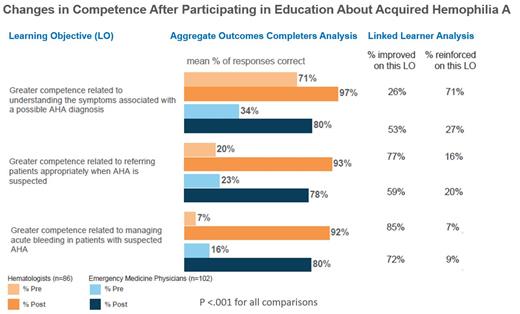
Overall significant improvements at the aggregate level were seen after participation for hematologists (33% average correct response rate at pre-assessment vs 94% at post-assessment; P<.001, Cohen's d= 2.27, N=86), and EM physicians (24% average correct response rate at pre-assessment vs 80% at post-assessment; P<.001, Cohen's d= 1.30, N=102). Highly significant improvements were achieved with regards to recognizing symptoms of AHA, appropriate referral, and initial therapeutic management (figure). After participating, 37% of hematologists and 40% of pulmonologists had measurable improved confidence (both P<.001), resulting in 63% of hematologists and 46% of EM physicians who were mostly or very confident in identifying features consistent with a possible AHA diagnosis post-CME (vs 44% and 26% pre-CME respectively).
CONCLUSIONS
This study demonstrates the success of online, interactive case-based education in improving clinicians' competence in identifying patients with possible AHA, appropriate referral and initial treatment. Both improvement and reinforcement in the context of a linked learning assessment have been shown to positively correlate with increases in confidence as well as intention to make clinical practice changes (Lucero KS, Chen P. J Eur CME. 2020 Oct 12;9(1):1834759), suggesting that most clinicians who participated in this activity are likely to make improvements in their practice. This could lead to earlier appropriate treatment and improved overall outcomes for these patients.
Ma: Takeda: Honoraria, Research Funding; Accordant: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal